Antibiotic resistance is a growing global challenge, particularly for modern healthcare, which relies on antibiotics to prevent and treat infectious diseases. Multi-resistant bacteria are already present across the globe and without effective antibiotics, simple medical interventions will become risky in the future. Each year, several million deaths globally are associated with antibiotic resistance. With more and more drug-resistant microorganisms, one could expect an increase in research and development of new antibiotics or vaccines. However, in parallel with the growing global threat from antimicrobial resistance, or AMR as it is often called, the development rate of new antibiotics is instead decreasing. Reduced R&D also reduces the number of experts in the field, which in turn affects our society’s ability to develop new antibiotics.
Why is that so? One reason is that the return on investment is so low that many large pharmaceutical companies have scaled back or abandoned their development programs, resulting in a loss of expertise. The effort to slow down the development rate of antibiotic resistance requires us to save the most effective medicines for the most difficult cases, and this “stewardship” contributes to inhibiting the will to invest, as the companies are unable to count on any new “blockbuster” drugs.
The problem of access to effective treatment is global, and on September 26 this year, the UN General Assembly is organizing a high-level meeting on AMR. The political declaration published ahead of the meeting highlights, among other things, the need for mechanisms for funding research and development, the need for functioning collaborations between private and public actors, and the need for measures to deal with the growing lack of competence in the area.
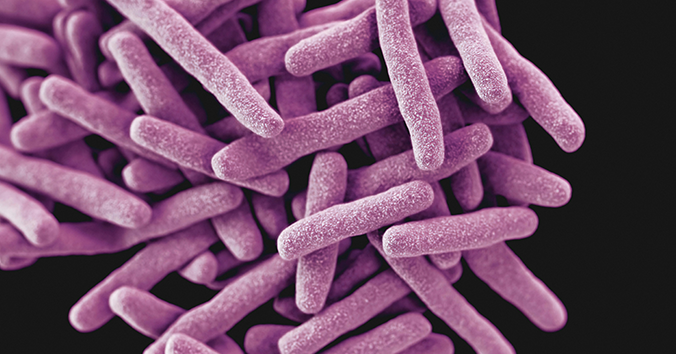
However, the picture is not only dark. During the last decade, several investments have been made in collaborations to meet the challenges for research and development in the field. One such investment is the European AMR Accelerator program, running since 2019 with funding from the Innovative Medicines Initiative (IMI). The program consists of nine projects that bring different stakeholders together to collaborate on the development of new treatments, for example against multi-resistant tuberculosis.
In a short article recently published in Nature Reviews Drug Discovery, representatives of the program discuss some of the important values and challenges associated with collaborations between academia and industry. Antibiotic development is expensive and many drug candidates are discontinued already in the early stages of development. By sharing risks and costs between several organizations, the AMR Accelerator has so far been able to contribute to the development of a large portfolio of different antibiotics. In addition, the nine projects have developed research infrastructures for, among other things, modelling, data management, and clinical studies that can benefit the entire AMR research community. Moreover, the critical mass that is generated when 98 organizations collaborate, can generate new ideas and synergies in the work against AMR.
There are also challenges. Among the challenges is balancing the perspectives and needs of different actors in the program, not least in the collaborations between academia and industry, where cooperation agreements and regular meetings have been needed to manage differences in culture and approach. The AMR Accelerator program has also served as neutral ground for competing companies, which have been able to can collaborate within the framework of the projects.
According to the authors, the biggest challenge remains: what happens after the projects end? The Innovative Medicines Initiative has invested €479 million in the program. The question now is how the nine projects and partners will find long-term sustainability for the assets and infrastructures they have put in place. Some form of continued funding is needed so that the resources created within the AMR Accelerator can be used in the next phase of the work, where the end goal is providing access to drugs that can treat antibiotic-resistant infections.
The article concludes with a call to governments, research funders, pharmaceutical companies and other actors to invest in research and development of new medicines and research to support the fight against antibiotic resistance. To ensure that we can benefit from investments such as the AMR Accelerator in the long term, regular funding calls are needed to maintain expertise, infrastructures, data and networks.
Read the highly topical article here: The AMR Accelerator: from individual organizations to efficient antibiotic partnerships.

Written by…
Pär Segerdahl, Associate Professor at the Centre for Research Ethics & Bioethics and editor of the Ethics Blog.
Fernow J, Olliver M, Couet W, Lagrange S, Lamers MH, Olesen OF, Orrling K, Pieren M, Sloan DJ, Vaquero JJ, Miles TJ & Karlén A, The AMR Accelerator: from individual organizations to efficient antibiotic development partnerships, Nature Reviews Drug Discovery, first online 23 September, DOI: https://doi.org/10.1038/d41573-024-00138-9
Approaching future issues







Recent Comments