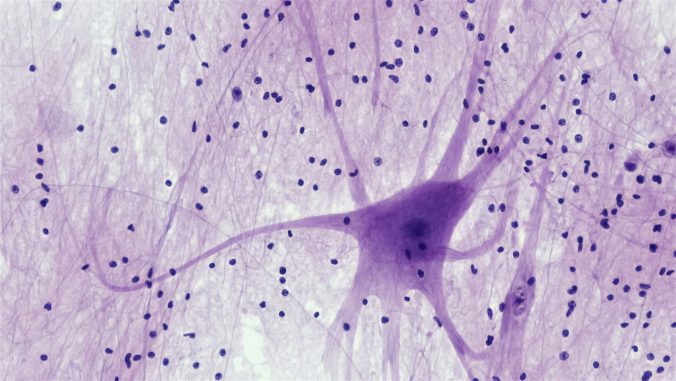
Multiple sclerosis (MS) is a chronic inflammatory disease that affects the nerves of the brain and spinal cord. Symptoms can vary between individuals and the progression of the disease is difficult to predict. Medications can slow the progression of the disease and relieve symptoms, but they do not cure the disease. Symptoms tend to come […]
Continue readingEvery day, researchers receive a motley of offers from dubious journals to publish in them – for a fee. The fact that researchers do not accept these offers does not prevent them from one day discovering that they have become authors of an article that they never wrote. This recently happened to four surprised colleagues […]
Continue readingAuthorities and researchers have a responsibility to the public to disseminate information about risks identified through research. Dissemination of information and education are also an important part of public health efforts to influence norms about lifestyle habits and support individuals in making informed choices about their health. Research has found links between overweight and at […]
Continue readingA large proportion of pregnant women in Sweden undergo prenatal diagnosis to assess the likelihood of chromosomal anomalies in the fetus. This initially involves a so-called CUB test, which combines ultrasound with a biochemical test. If the CUB test indicates a high probability of a chromosomal anomaly, further tests are offered. This can be a […]
Continue readingHow do you handle a reluctant patient who may not want to take their medication or who protests against measures that are deemed to be beneficial to the patient, such as inserting a urinary catheter? Do you just give up because the patient does not consent? Except in acute emergency situations, coercive somatic treatment is […]
Continue readingMost people are probably aware that antimicrobial resistance is one of the major threats to global health. When microorganisms develop resistance to antibiotics, more people become seriously ill from common infections and more people will die from them. It is like an arms race. By using antibiotics to defend ourselves against infections, we speed up […]
Continue readingWhy is the question of truth so marvelous? A common attitude is that the question can make us check that our opinions really are correct before we express them. By being as well-informed as possible, by examining our opinions so that they form as large and coherent a system as possible of well-considered opinions, we […]
Continue readingIndividuals with borderline personality disorder (BPD) often suffer from strong emotions that change rapidly, from one extreme to another. They may fear abandonment and experience an inner emptiness. They may also behave impulsively and have suicidal thoughts or behaviors. BPD is often mis- or underdiagnosed and there is a tendency among clinicians to avoid the […]
Continue readingIn palliative care of seriously ill and dying patients, healthcare professionals deal not only with medical needs, but also with the existential needs of patients and their families. Although the palliative healthcare teams can receive support from professions that focus on existential conversations, it is the physicians and not least the nurses, care assistants, physiotherapists […]
Continue readingMany healthcare professionals who work in nursing report that they experience a sense of dehumanization in their work. Although this is an increasingly recognized problem, it is still unclear how it manifests itself in practice and should be addressed. Previous studies indicate that the experience of dehumanization is often linked to excessive workload, lack of […]
Continue reading










Recent Comments