Life always surpasses us. We thought we were in control, but then something unexpected happens that seems to upset the order. A storm, a forest fire, a pandemic. Life appears as a drawing in sand, the contours of which suddenly dissolve.
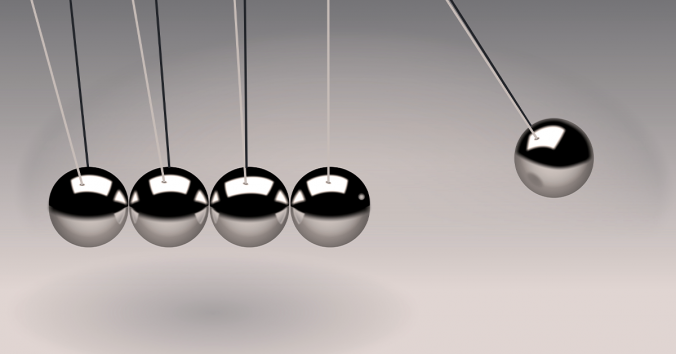
Of course, it is not that definitive. Even a storm, a forest fire, a pandemic, will pass. The contours of life return, in somewhat new forms. However, the unexpected reminded us that life is greater than our ability to control it. My question in this post is how we balance the will to control life against the knowledge that life always surpasses us.
That life is greater than our ability to control it is evident not only in the form of storms, forest fires and pandemics. It is evident also in the form of nice varying weather, growing forests and good health. Certainly, medicine contributes to better health. Nevertheless, it is not thanks to any pills that blood circulates in our bodies and food becomes nourishment for our cells. We are rightly grateful to medicine, which helps the sick. However, maybe we could devote life itself a thought of gratitude sometimes. Is not the body fantastic, which develops immunity in contact with viruses? Are not the forests and the climate wonderful, providing oxygen, sun and rain? And consider nature, on which we are like outgrowths, almost as fruits on a tree.
Many people probably want to object that it is pointless to philosophize about things that we cannot change. Why waste time reflecting on the uncontrollable dimensions of life, when we can develop new medicines? Should we not focus all our efforts on improving the world?
I just point out that we then reason as the artist who thought himself capable of painting only the foreground, without background. As though the background was a distraction from the foreground. However, if you want to emphasize the foreground, you must also pay attention to the background. Then the foreground appears. The foreground needs to be embraced by the background. Small and large presuppose each other.
Our desire to control life works more wisely, I believe, if we acknowledge our inevitable dependence on a larger, embracing background. As I said, we cannot control everything, just as an artist cannot paint only the foreground. I want to suggest that we can view philosophy as an activity that reminds us of that. It helps us see the controllable in the light of the uncontrollable. It reminds us of the larger context: the background that the human intellect does not master, but must presuppose and interact with wisely.
It does not have to be dramatic. Even everyday life has philosophical dimensions that exceed our conscious control. Children learn to talk beyond their parents’ control, without either curricula or examinations. No language teacher in the world can teach a toddler to talk through lessons in a classroom. It can only happen spontaneously and boundlessly, in the midst of life. Only those who already speak can learn language through lessons in a classroom.
The ability to talk is thus the background to language teaching in the classroom. A language teacher can plan the lessons in detail. The youngest children’s language acquisition, on the other hand, is so inextricably linked to what it is to live as a human being that it exceeds the intellect’s ability to organize and govern. We can only remind ourselves of the difference between foreground and background in language. Here follows such a philosophical reminder. A parent of a schoolchild can say, “Now you’ve been studying French for two hours and need a break: go out and play.” However, a parent of a small child who is beginning to talk cannot say, “Now you’ve been talking for two hours and need a break: go out and play!” The child talks constantly. It learns in the midst of playing, in the midst of life, beyond control. Therefore, the child has no breaks.
Had Herb Terrace seen the difference between foreground and background in language, he would never have used the insane method of training sign language with the chimpanzee Nim in a special classroom, as if Nim were a schoolchild who could already speak. Sometimes we need a bit of philosophy (a bit of reason) for our projects to work. Foreground and background interact everywhere. Our welfare systems do not work unless we fundamentally live by our own power, or by life’s own power. Pandemics hardly subside without the virus moving through sufficiently many of our, thereafter, immune bodies – under controlled forms that protect groups at risk and provide the severely ill care. Everywhere, foreground and background, controllable and uncontrollable, interact.
The dream of complete intellectual control is therefore a pitfall when we philosophize. At least if we need philosophy to elucidate the living background of what lies within human control. Then we cannot strive to define life as a single intellectually controllable foreground. A bit of philosophy can help us see the interplay between foreground and background. It can help us live actively and act wisely in the zone between controllable and uncontrollable.

Written by…
Pär Segerdahl, Associate Professor at the Centre for Research Ethics & Bioethics and editor of the Ethics Blog.
We like ethics